Dissociation: A Case Study
Dissociation and/or Multiplicity – A Case Study By Alana Roy
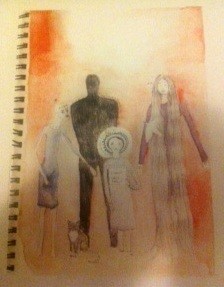
When I first began my social work career at a rape crisis centre, I had the privilege of working alongside a 25-year-old woman called Emma. Emma was referred to me for counselling due to childhood trauma. We engaged in weekly therapy sessions for two years. Over the course of the therapy, Emma revealed a complex and fascinating survival system (DID) that developed due to the horrific sexual abuse she had experienced by a family member from the age of three. Emma gave me permission to use her art and journal entries to help educate others about Dissociative Identity Disorder (DID). The pictures below display Emma’s system, and provide examples of how she began to make connections within her dissociative system.
Emma had been given various diagnoses such as borderline personality disorder, depression, anxiety, PTSD, psychotic episodes, and anorexia and bulimia. Emma reported a range of terrible experiences within the mental health system and felt as though she had not been understood. Emma had not been able to explore her trauma, and survival skills in a safe therapeutic environment. In addition, Emma was taking a multitude of medications and lost track of her specific diagnosis and the side effects of the tablets. When working with Emma it became evident that she was experiencing dissociation. I used a range of therapies such as feminist counselling, emotion focused therapy and a specific “trauma model” by Dr Colin Ross to guide practice. In addition, art and writing became central to Emma’s expression and healing processes. Together, we developed a range of treatment goals that are helpful with complex dissociative disorders.
Stage 1 involved developing trust in the therapeutic relationship, establishing emotional and physical safety, psycho education about co?morbidity and dissociation, overcoming dysregulation and slowly allowing Emma to remember the trauma without reliving it and being re-traumatised. Stage 2 involved reconstructing her traumatic narrative, establishing communication within her system, orienting the body to present moment, problem solving and goal setting as a system, and the teaching and practicing of new self soothing skills. Stage 3 involved Emma slowly emerging as a more connected person and system, the practising of safety, self-soothing and relationship building and connecting with the community.
I will attempt to summarise the main elements of her system, but this is only a very brief outline of the amazing survival system that Emma has. Please refer to the pictures attached that Emma designed to express her system.
Emma identifies as being the “host personality”, the one who is “out” the majority of the time. Emily is the spiritual part of Emma who is very creative, protective and sensitive. Together, Emma and Emily created a “nest” in her mind. They go to the nest to “rest and sleep” when the trauma memories became too hard to manage.
Anna (8 years) and is a child part who is aware of some of the abuse that occurred but exists to protect a smaller child part. Sally is 3 or 4 years and is silent unless with Anna. Sally holds most of the abuse memories. During therapy Anna and Sally became less frightened. Adult Emma and her spiritual part provided comfort, and protection to these fearful, and traumatised parts.
D is 12 and 14 years old. This part experiences black and intense depression and can have an abusive voice. D kept the entire system silent during early teenage years. D also has the ability to be aggressive and protect the entire system if under threat. As the therapy progressed D became significantly less angry; D became assertive and protective. Although D still experienced depression that intensity of the depression reduced and Emma had a developed a range of strategies to help manage this.
Minna or M was identified as being 16 year old and the “sad, depressed and suicidal part”. Minna or M often engaged in self-harming behaviours, substance abuse, suicide attempts, and experienced eating disorders. Mina was identified as the shift from internalising emotions to actually “acting out” the anger and rage. Mina is like a rebellious teenager that rejects authority. During the therapy process Emma was able to place her adult self along side this rebellious part to help reduce impulsivity, self harm and to provide acceptance and support. Overall Emma impulsivity and sense of shame significantly reduced.
I spent a challenging and inspirational two years working alongside Emma and her survival system. When our counselling finished Emma had developed safety, and a deep insight into her dissociative system. Emma no longer took a range of medications or identified with the variety of diagnosis that she had been given. Emma can now see that her illness is something to be understood and respected. When I moved interstate, Emma wrote to me on a good bye card saying “ I may have further to go on my journey but I now have trust and respect for myself as a person, I have learnt so much about myself and my sickness and I have grown and healed in ways I could never imagine”.
When I reflect on my time working at rape crisis centre and all the women I worked with who experienced dissociation and or multiplicity I wish I could have referred them to a specialist support group. When I finished working with Emma she had began to live as a more connected person and I strongly believe that she could have benefited from peer support; to share and learn from other people with similar experiences.
Sue Nunn and I have developed “Echoes” a peer support group for those who experience dissociation and or multiplicity. Sue highlights below the importance of peer support groups.
 Peer support is based on giving and receiving help founded on key principles of respect, shared responsibility, and mutual agreement of what is helpful. Peer support is not based on psychiatric models and diagnostic criteria. It is about understanding another’s situation empathically through the shared experience of emotional and psychological pain. When people find affiliation with others they feel are ‘like’ them, they feel a connection. This connection, or affiliation, is a deep, holistic understanding based on mutual experience where people are able to ‘be’ with each other without the constraints of traditional expert/patient relationships. Echoes is a Peer Support group based on these principles it provides people a supportive learning environment in which to develop the skills, understandings, attitudes and strategies to improve mental wellbeing. It provides a much-needed resource for those of us who are still being met with the denial by the psychiatric system that our condition Dissociative Identity Disorder doesn’t exist.
Peer support is based on giving and receiving help founded on key principles of respect, shared responsibility, and mutual agreement of what is helpful. Peer support is not based on psychiatric models and diagnostic criteria. It is about understanding another’s situation empathically through the shared experience of emotional and psychological pain. When people find affiliation with others they feel are ‘like’ them, they feel a connection. This connection, or affiliation, is a deep, holistic understanding based on mutual experience where people are able to ‘be’ with each other without the constraints of traditional expert/patient relationships. Echoes is a Peer Support group based on these principles it provides people a supportive learning environment in which to develop the skills, understandings, attitudes and strategies to improve mental wellbeing. It provides a much-needed resource for those of us who are still being met with the denial by the psychiatric system that our condition Dissociative Identity Disorder doesn’t exist.
The isolation that is felt by someone who has a dissociative disorder is crippling and a lot of people with DID struggle to believe that they have DID. They struggle to believe that they had a traumatic history and they struggle to believe that the plethora of symptoms which plague their lives on a daily basis are anything other than a sign that they are intrinsically ‘bad’ or hopelessly ‘mad’. Many of us with DID hate our diagnosis, are deeply ashamed of it and as a result don’t want anyone else to know about it. Echoes is the only Peer Support group for people with dissociative experiences that exists in Melbourne.
Alana Roy is a Emotion Focused Mental Health Social Worker who works in the field of sexual assault and complex trauma. Alana uses EFT to help people understand, tolerate, experience, and transform emotions safely. Alana is dedicated to creating more awareness and acceptance of those who experience dissociation and/ or multiplicity. Register now for a presentation on Tuesday, June 26 (6:30-7:30 pm) to learn more about Dissociative Identity Disorder and how Echoes helps people to share, listen, feel heard, and develop strategies to better manage dissociative experiences.